When improving health requires patients to change behavior, virtual humans help providers get results.
Contributor: Antoinette M. Schoenthaler, EdD
Healthcare providers can do everything “right”—the right diagnosis, the right treatment plan, the right follow-up care—but if patients don’t take an active role in their health, they likely won’t achieve optimal results.
Getting patients on board, especially when a change in attitude or behavior is required to see lasting health outcomes, requires effective communication between healthcare professionals and patients. It’s no secret that strong soft skills are in high demand in the healthcare industry, but soft skills training is often ineffective, expensive, or even absent in some facilities. A new trend is helping fill this gap: Through the power of simulation technology and virtual humans, healthcare professionals are gaining conversation skills that could make a life-saving difference for their patients.
 Simulation training addresses critical skills gaps
Simulation training addresses critical skills gaps
Healthcare educators and employers providing continuing education often lean on the use of role-play with standardized patients to help current and future healthcare professionals develop skills like Screening, Brief Intervention, and Referral to Treatment (SBRIT); motivational interviewing; and empathy. However, these sessions can require a great deal of time and resources, are difficult to standardize, and make some participants uncomfortable. Online simulation training is a solution growing in popularity because of its effectiveness, its ability to standardize, and its easy-to-access digital medium.
Antoinette M. Schoenthaler, EdD, is a behavioral scientist and an associate professor of public health and medicine at New York University (NYU). She has helped lead studies determining the effectiveness of simulation training in primary care settings. As someone who also leads in-person workshops, she says that one of the unique advantages to simulation training over a traditional, in-person role-play is the one-on-one feedback provided.
“Oftentimes for providers, we are offering two- to three-hour workshops, which can be good, but it really results in just gaining knowledge. It’s not really skill acquisition,” Schoenthaler says. “As a trainer, it’s very hard for me to give good, constructive feedback when I have 35 people in the room, because there’s only so much time I can dedicate to each person. [Online] simulation [training] provides a really good opportunity to get that one-on-one feedback.”
Hospitals, primary care offices, state and local agencies, and schools of health professions are implementing these trainings to help improve conversations that can positively impact a variety of patient outcomes (see chart below). Most of these simulations are used to train future and current healthcare professionals, but simulations can also be designed for patient education. For example, in a simulation developed in partnership with the Robert Wood Johnson Foundation, patients learn how to navigate conversations with their providers about topics such as antibiotics overuse. There is also an online simulation and mobile app funded by the CDC called “Talk to Someone.” In this app, triple negative breast cancer (TNBC) patients can better understand their diagnosis and the advantages of chemotherapy by engaging with “Linda,” a virtual TNBC survivor.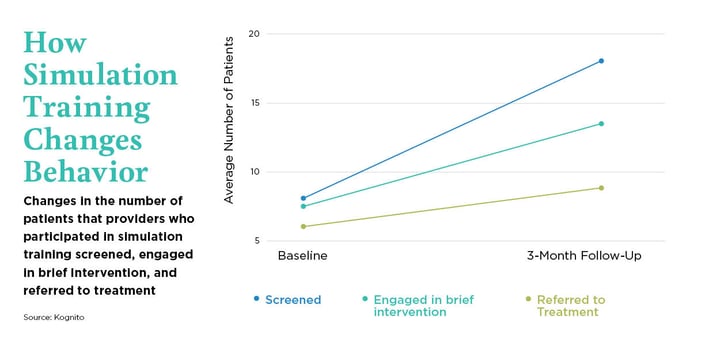
The advantage of virtual humans
In some methods of simulated training, such as those described above, participants role-play with virtual humans. They can experiment with different clinical approaches and communication styles without fear of repercussions to real patients or discomfort from role-playing with an actor or peer. Studies show that students and medical professionals who engage with virtual humans feel more prepared to manage health conversations effectively. They also report feeling more safe in a risk-free environment, less judged, and more willing to reveal information honestly.2,3,4
The right level of realism in appearance, responses, and verbal and non-verbal communication can give virtual humans the power to help healthcare professionals practice in a safe environment without the risk of embarrassment or actual patient repercussions. The degree to which they are human-like is very intentional so that the user doesn’t get distracted by them and start associating them with someone they know rather than focusing on the training content. In fact, the best retention, engagement, and overall learning is achieved when virtual humans are not overly realistic.5,6 Research also suggests that users are more open to receiving feedback from a synthetic agent than from a human being, another advantage of virtual humans in simulation technology.7
 Is virtual simulation training improving quality of care?
Is virtual simulation training improving quality of care?
Simulation training is helping healthcare providers and clinical professionals—and patients—gain confidence in their ability to lead meaningful conversations. But does increased confidence in conversation skills lead to real results?
Kognito is the leading developer of health education simulations. Their evidence-based approach creates virtual human role-play training aimed at improving confidence and conversation skills. They combine the art of conversation with the science of learning, such as implementing the dual coding theory—balancing the visual with auditory learning equally to address different learning styles. The company has several simulations for healthcare professionals regarding topics such as substance use disorders and mental health concerns.
Various studies determining the effectiveness of Kognito’s simulation training have shown statistically significant changes in the frequency by which healthcare professionals initiated the intended health conversation. Healthcare professionals were also shown to implement research-backed communication strategies more often.8 Below are highlights from a few of these studies.
In a simulation designed to help pediatricians and other health professionals have conversations with parents and their children about healthy weight and childhood obesity, 93% of users reported that as a result of the training, they intended to make a change in practice to provide better patient care.6
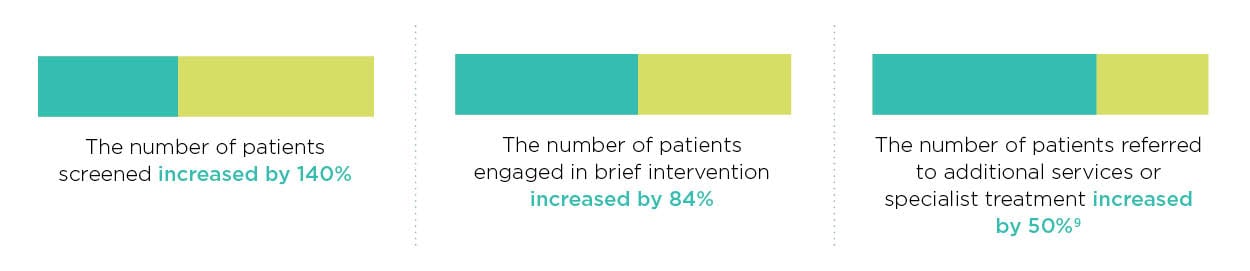
77% of physicians who completed a simulation aimed at helping them lead conversations with patients about the proper use of antibiotics said it had a positive impact on the way they communicate with patients.6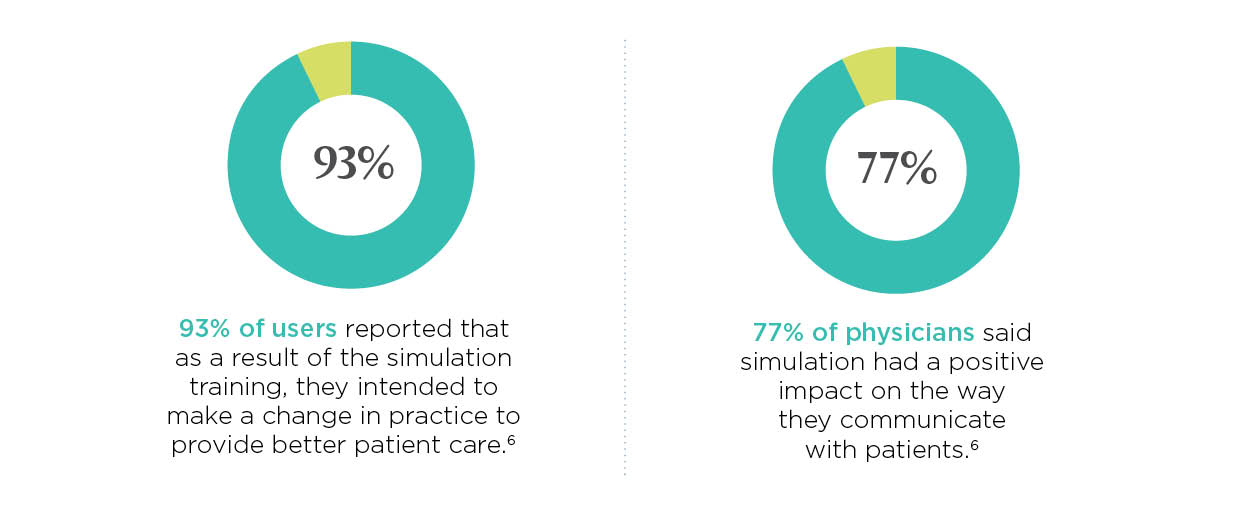 After completing a simulation designed to help providers screen patients for substance use and mental health disorders, providers increased the number of patients screened by 140%, engaged 84% more patients in brief intervention, and referred nearly 50% more patients to additional services or specialist treatment.9
After completing a simulation designed to help providers screen patients for substance use and mental health disorders, providers increased the number of patients screened by 140%, engaged 84% more patients in brief intervention, and referred nearly 50% more patients to additional services or specialist treatment.9
By practicing conversation skills with virtual humans, healthcare providers can learn in a comfortable environment. Virtual role-play allows them to gain confidence in their ability to have productive conversations with patients surrounding difficult topics and to do so at a higher frequency.
Additional research is in process to look at the role of simulation in impacting long-term health outcomes of the patients who are on the other side of these conversations. However, the initial results indicate optimism in improving the dialogue and soft skills of healthcare professionals to help them better serve their patients’ needs—even when those needs are outside of the medical professional’s scope of practice.
Schoenthaler says that as patient-centered care becomes the norm, current and future medical professionals must have access to training to improve patient communication. “We have to think out of the box for training providers, healthcare professionals and even patients in how to communicate better,” she says. “Any way that we can get people more exposure is really important.”
References
-
Center for Substance Abuse Treatment. Enhancing Motivation for Change in Substance Abuse Treatment. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 1999. (Treatment Improvement Protocol (TIP) Series, No. 35.) Chapter 3—Motivational Interviewing as a Counseling Style. Retrieved on January 28, 2020 from: https://www.ncbi.nlm.nih.gov/books/NBK64964/
-
Lucas, G. M., Gratch, J., King, A., & Morency, L. P. (2014). It’s only a computer: Virtual humans increase willingness to disclose. Computers in Human Behavior, 37, 94-100.
-
Rizzo A, Scherer S, DeVault D, et al. (2016). Detection and computational analysis of psychological signals using a virtual human interviewing agent. Journal of Pain Management. 9:311-21.
-
Pickard, M. D., Roster, C. A., & Chen, Y. (2016). Revealing sensitive information in personal interviews: Is self-disclosure easier with humans or avatars and under what conditions? Computers in Human Behavior, 65, 23-30.
-
Mori, M., MacDorman, K. F., & Kageki, N. (2012). The uncanny valley [from the field]. IEEE Robotics & Automation Magazine, 19(2), 98-100.
-
MacDorman, K. F., Green, R. D., Ho, C. C., & Koch, C. T. (2009). Too real for comfort? Uncanny responses to computer generated faces. Computers in human behavior, 25(3), 695-710.
-
Lowes, S., Hamilton, G., Hochstetler, V., & Paek, S. (2013). Teaching communication skills to medical students in a virtual world. Journal of Interactive Technology and Pedagogy (3).
-
Albright G, Adam C, Serri D, Bleeker S, Goldman R. Harnessing the power of conversations with virtual humans to change health behaviors. mHealth 2016;2:44.
-
Albright, G. & Adam, C. (2018). At-Risk in Primary Care: A Longitudinal Study with 877 Health Professionals. Kognito. Retrieved on January 28, 2020 from https://go.kognito.com/rs/143-HCJ-270/images/Healthcare_PCP_KognitoResearch_2018.pdf