For current NHA certification holders, log into your NHA account and complete the CE activity associated with this article.
Continuing Education Objectives
- Describe how electronic health records (EHRs) grew in prominence.
- Identify the positive effect EHRs have had on healthcare.
- Define some of the common errors and challenges when using an EHR.
- List strategies and solutions to combat errors, avoid burnout, improve information sharing, and protect patient privacy.
- Describe what will shape the future of EHR.
Electronic health records (EHRs) were touted as a pathway toward better, safer, and more inexpensive healthcare, but a look back shows improvements have been slow, often due to technology issues. While the complex array of EHR options still poses challenges, one route toward better utilization is improving how humans interact with EHRs.
Evolution of EHRs
In 2004, the U.S. government set a 10-year goal for all healthcare organizations to be using EHRs to help avoid medical errors, reduce costs, and improve patient care. Efforts to develop the EHR represented a long journey from early visions to today’s reality, where EHRs have been adopted across the majority of hospitals and physicians practices throughout the U.S.
The EHR is not a simple computer application; rather, it represents a carefully constructed set of systems that are highly integrated and require a significant investment of time, money, process change, and human factor reengineering.
Effect of EHRs on healthcare
Depending on who you talk to, EHRs have had a positive effect, very little effect, or a negative effect on healthcare. Some patients and providers prefer communicating electronically. Some patients hate that their provider spends most of the visit looking at the computer, entering data, and spending too little time on personal interaction.
While noting that it is too soon to determine whether the significant time spent by interns with electronic records is a misuse of time, Krisda Chiayachati, M.D., an assistant professor of Medicine in the Perelman School of Medicine of the University of Pennsylvania, believes that “indirect patient care has tradeoffs.” She adds, “If it takes time away to the point that the patient feels like we aren’t listening to their needs or we lose out on human interactions that provide physicians with a sense of purpose, that is a bad thing. But if it helps us diagnose diseases more efficiently, then maybe that’s not that bad in the end.”1
The obvious goals of the EHR are to improve patient safety, improve quality care, and reduce healthcare costs. So, where is the industry at today when it comes to the EHR?
Positive effects
While EHRs are continually evolving and improving, most users agree that transitioning from paper to electronic health records has saved countless lives. Access to complete and accurate patient information has had a number of positive effects:
- Improved patient care
- Increased patient participation
- Improved care coordination
- Improved diagnostics and patient outcomes
- Practice efficiencies and cost savings2
Consider the effect of poor communication and illegible handwriting in paper records. As connectivity and interoperability of EHRs improve, so will healthcare overall. From a provider’s perspective, Blake Busey, D.O., a family practice physician who works at Texas Tech University Health Sciences Center in El Paso, Texas, describes some of the positive effects he has experienced using the EHR:
- Legible notes and clear documentation allow for decreased ambiguity and miscommunication.
- Electronic ePrescribing decreases the time spent writing prescriptions.
- Quick text, dictation software, and macros allow for better capture of information.
- De-identified data mining allows access to data for research and quality efforts.3
Challenges
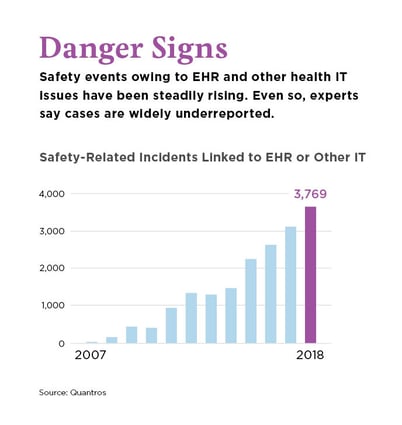
In 2019, the ECRI Institute, a non-profit organization focused on cost-effective patient care, reported that “diagnostic errors and improper management of test results” topped the list of EHR-related patient safety concerns. Part of the reason for concern is that “when diagnoses and test results are not properly communicated or followed up on, the potential exists to cause serious harm or death.”4
Providers are busy and they want EHRs that make their lives easier, not more complicated.5 Expanding on this point, Dr. Busey cites additional challenges providers experience.
Quality of communication
Dictation can cause errors such as nonsensical information that is phonetically correct.
Software failures
Technology glitches can lead to downtime, which leads to paper charting.
Interoperability issues
Information cannot always be shared electronically across various providers, and health systems may not have the same EHR program. While there has been great progress in interoperability in the last decade, EHRs are not always interconnected, leading to faxed records and more paper.
Poor-quality systems
EHRs are expensive, so employers may choose more inexpensive or lower-quality products to save cost. Poor-quality EHRs are one of the leading reasons for physician burnout.
Billing issues, upcoding, and fraud
Use of quick texts will often lead to upcoding and potentially overbilling. Insurance providers require more documentation (and thus time) to justify payment and prior authorizations.3
Copy/Paste
Copy/paste, also known as cloning, has been identified as a challenge by the Office of Inspector General (OIG). Providers will copy documentation from a previous encounter and paste the documentation into a current note without updating the record.18
Other concerns include privacy and HIPAA compliance. Personal, face-to-face communication between provider and patient can also be inhibited by how the provider uses the EHR.
Common errors using the EHR
When using the EHR, both human and technology factors affect the ability to accomplish the goals of increasing safety, improving quality of care, and reducing cost.
The human factor
Humans make mistakes. Data entry issues, such as selecting a wrong CPT or ICD-10 code, entering the wrong dosage and instructions on a medication, failure to communicate with patients in the patient portal, or neglecting to schedule a required patient follow-up, can be life-altering mishaps.
Lack of follow-up on orders/results
While EHRs have created systems that allow quick transfer of information, workflow issues can still create problems in terms of properly handling critical information. For example, when test results are received in the EHR, proper workflow is required to ensure that the results are addressed: the physician reviews the results, the patient receives notification, and any follow-up tests or visits are scheduled.
Failure to communicate with patients
Most EHRs have a patient portal feature allowing the patient to communicate with the provider, see results, and request refills. When patients make requests, prompt attention is required from staff members to process the information and facilitate any next steps. Many internal messaging applications require staff to enter a significant amount of detailed and accurate information, which then needs to be communicated to both the provider(s) and the patient. The EHR cannot solve for the human factor of communication to patients, but it can be designed to include prompts and safeguards.
The technology factor
Despite the best of intentions, not all EHRs are easy for providers to use and for IT departments to maintain. The frequency of updates and how providers can navigate between screens can affect proper usage. Because of these and many other factors, there are a number of common mistakes hospitals and other healthcare workers make with EHRs.
Autocorrect and autofill functionality can cause errors. This technology is useful in other applications, but when it happens in an EHR, it can result in the wrong medication name or dosage, an incorrect diagnosis, or the addition of other medical information without anyone noticing an error. To combat these errors, start by turning off or modifying these features and reviewing workflow processes that may currently require unnecessary steps, forced clicks, or other inefficiencies.6 You can improve efficiency, reduce wasted time, and decrease burnout by continually optimizing the EHR based on regular reviews of workflows.
User experience
For people who have worked in healthcare for more than 20 years, the EHR has transformed the daily experience—from how they interact with patients and each other, to how they obtain critical information to ensure patients receive the care they need at the right time. Perspectives on the benefits and challenges of working in the EHR vary based on roles and responsibilities.
Provider experience
Although intended as a timesaving tool that improves patient care and reduces errors and costs, the EHR requires about the same investment in time as paper records, and it’s expensive. Constant updates and upgrades to the EHR require more training and contribute to provider burnout. The ECRI Institute notes that “keeping up with the changes can be a challenge” and “time pressures are intense. Providers are caring for an increasing number of patients with complex medical conditions, drawing on limited resources.”7 Many providers have left the profession rather than take on the cost and task of learning new electronic programs.
Support staff experience
EHRs have transformed workflows for support staff. For example, organizations with EHR systems that interface with partnering labs can have results automatically loaded into the EHR. Many prescriptions no longer need to be called into the pharmacy; providers can send them to the pharmacy electronically while the patient is in the office. This has saved time for support staff like medical assistants.
A KLAS Research survey of 28,000 nurses found them to be more satisfied than providers with EHRs (62% report they are pleased), but there is still room for improvement, especially when it comes to integration with outside organizations.8
Patient experience
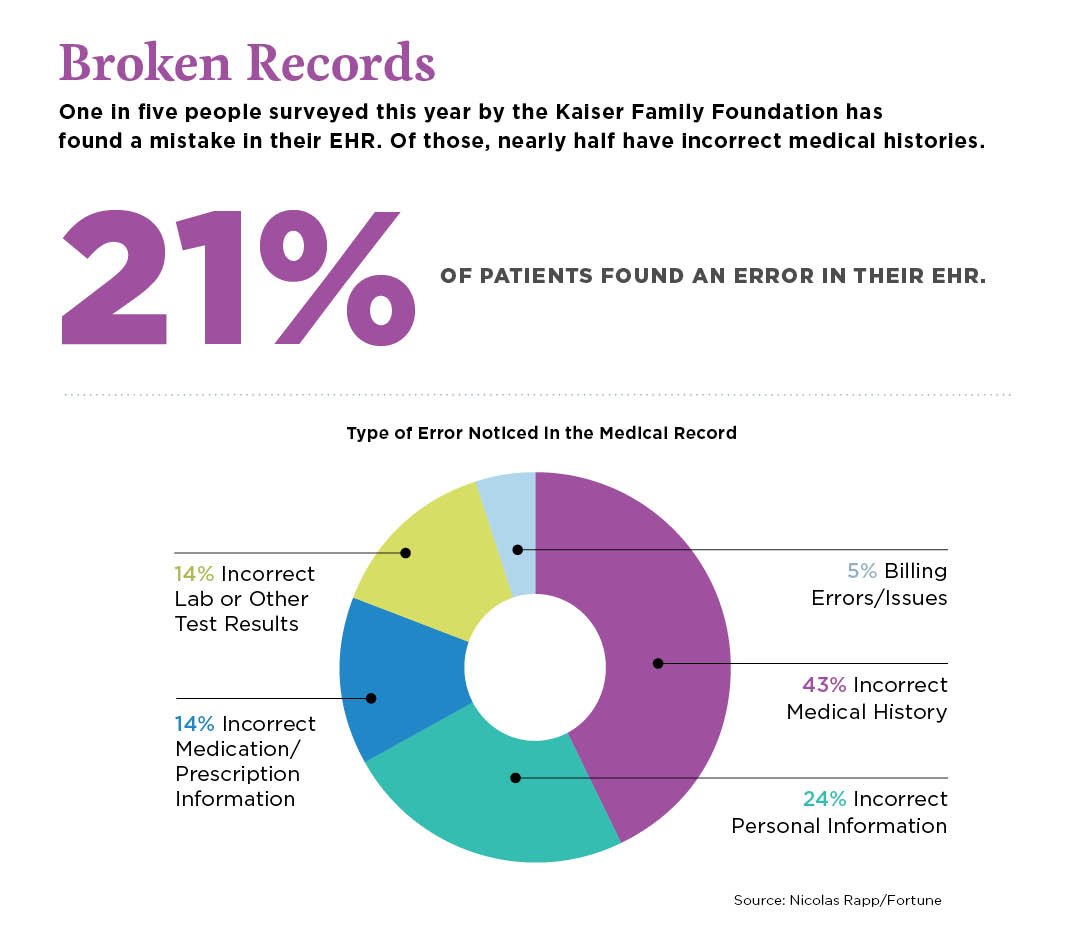
In 2019, the Kaiser Family Foundation reported that about 45% of patient respondents think the EHR has improved the quality of care and interactions with physicians. Roughly half of patients are concerned about unauthorized access to their records or errors that could affect their care; 21% report that they or a family member have discovered an error in their EHR.9
During interviews with patients, many expressed appreciation of features of the EHR, such as viewing results of tests, making in-person appointments, and arranging phone or video appointments. However, patients report dissatisfaction with EHR glitches, such as receiving electronic notifications for being late on blood work, being asked repetitive questions, and allergies or medication interactions not being updated. All patients interviewed expressed frustration with the amount of time the provider spent on the computer instead of face-to-face interaction during the visit.10
 Strategies and solutions
Strategies and solutions
A key to improving satisfaction with EHRs is to avoid getting trapped behind technology, as this is one of the patients’ biggest complaints. From the provider perspective, Dr. Busey suggests the following:
- Purchase a high-quality EHR that works for the practice; it costs more to recruit, hire, and onboard new physicians than to buy appropriate software.
- Ensure that implementation and service are part of the contract agreement with the vendor.
- Implement a regular peer review to bring coders and support staff together for the purpose of quality review.3
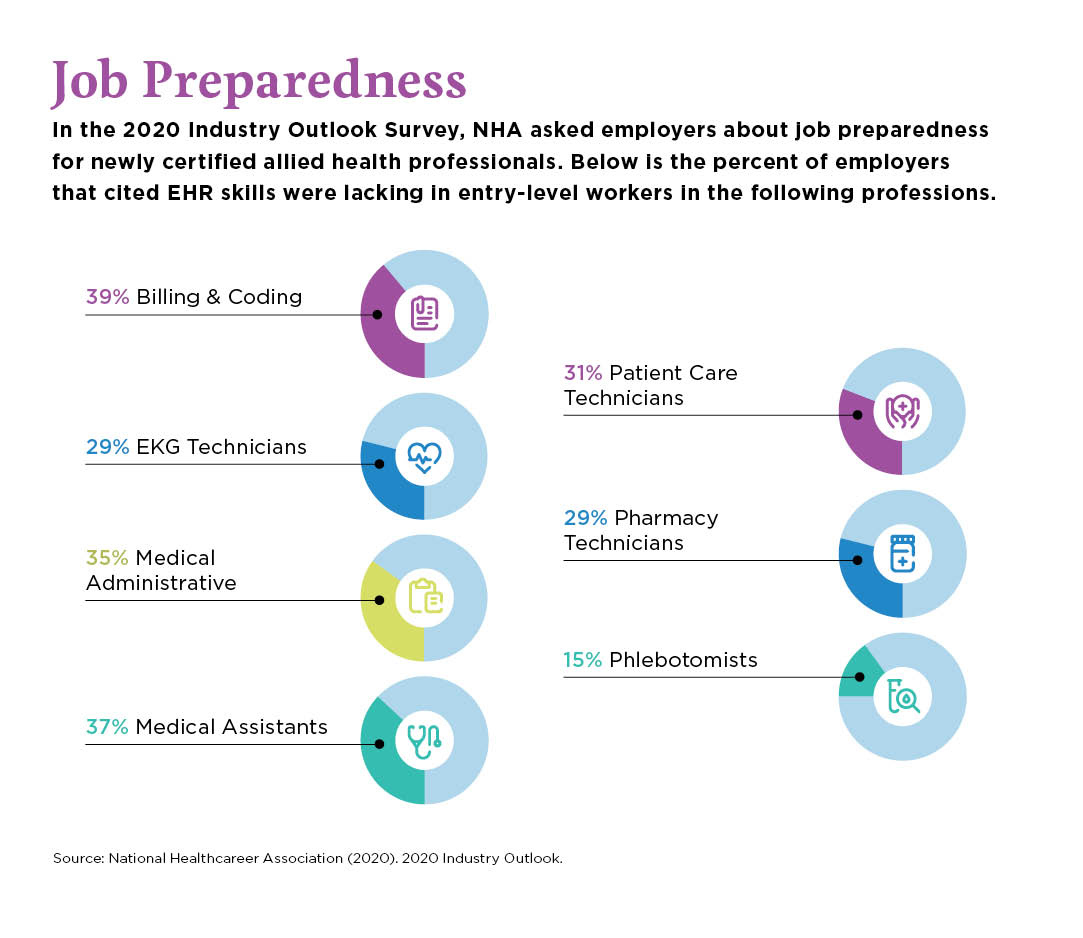
Improving the providers’ user experience can increase satisfaction, quality, and accuracy. To prevent frustration with the EHR, ensure that your selected EHR integrates with external organizations. Make sure to purchase a certified EHR program to ensure that bonus incentives can be obtained by insurance carriers, such as Medicare. Also, conduct training and encourage certification for all members of the team who will interact with the EHR. As you develop your EHR training, consider how to build strong mechanics while ensuring that EHR users understand the underlying importance of the EHR, what critical healthcare processes it drives, and how their actions can impact patients, operations, and revenue reimbursement.
Combatting human errors
To improve employee engagement, Kenneth Longbrake, MSN, RN, CPEN, suggests conducting quarterly employee engagement surveys to evaluate the EHR product and usage so the team can create action plans.11
While many EHRs are similar, there are distinct differences. Organizations must provide initial and ongoing training for providers, support staff, and others. Some organizations develop training materials in-house and offer live training sessions. Management can identify superusers in these training sessions and give the superusers the opportunity to mentor and train others to properly use the EHR.
The EHR provides an audit trail, or a digital footprint, of every user and every keystroke, which means there’s ample opportunity to identify errors that can be used for learning and training. Leadership and users should work together to identify errors, determine the root cause, and recommend corrective action. By treating errors as opportunities for improvement, leadership creates a culture that prioritizes patient safety, one of the ECRI Institute key recommendations.7
Avoiding EHR burnout
Burnout is common in healthcare. Ellen Deutsch, M.D., M.S., medical director of
the ECRI Institute, describes burnout as “morally exhausting,” resulting in decreased productivity. Dr. Deutsch suggests that health system administrators should gather feedback from providers and implement systemic changes.7
A contributing factor to burnout is the EHR and frustrations with documentation. According to a 2018 Merritt Hawkins survey, 78% of doctors suffered symptoms of burnout, and “other[s] [have] deemed it a ‘public health crisis.’”12
Burnout attributed to EHR fatigue can be avoided by ensuring all EHR users learn the program, expectations, rules, and guidelines. Providers benefit from being trained early in the hiring process, using voice recognition software or a scribe, and having a manageable login and password process. Short, frequently scheduled training sessions should address updates that impact users. Lastly, an internal superuser can serve as a champion and resource for the whole team.
Future of EHRs
In 2007, the Institute for Healthcare Improvement (IHI) introduced the “Triple Aim”:
- Improve individual patient experience
- Enhance population health
- Reduce healthcare costs
Because of the extent of burnout in the industry, the Triple Aim shifted to the Quadruple Aim, with the introduction of a fourth goal: improve staff satisfaction.13
Across healthcare, these goals continue to shape how organizations use EHRs. While there is broad commitment in the healthcare industry to achieve these goals, some challenges faced now will continue into the future.
The future of the EHR will be to integrate healthcare reimbursement and quality improvement. For example, there are a variety of payment mechanisms (healthcare payment models), but the effectiveness varies widely. Fee-for-service, for example, appears to be moving “toward ‘value-based care,’ because it ties reimbursement to metric-driven outcomes, proven best practices, and patient satisfaction, thus aligning payment with value and quality.”14
Experts agree that emerging health information technology (HIT), integrated with the EHR, shows promise to improve efficiency. According to John Britton, “optimal reimbursement for healthcare must account for not only the quantity of care provided but also the complexity and quality of that care.”15
Britton elaborates: “Any mechanisms to do so will require the accumulation, synthesis, and interpretation of information to guide renumeration while simultaneously enhancing the efficiency and quality of care. The ability of a well-designed and utilized EHR is ideally suited to play a central role in accomplishing this goal.”
Regulatory effects and challenges
According to Cerner Corporation, one of the largest EHR vendors, “the sheer size and rapid-fire release of regulations are nearly impossible to keep up with.”16 Many vendors offer contracts, including regulatory consulting services, to lead users through the future of regulatory compliance (e.g., HIPAA compliance).
Improving information sharing
Interoperability is a challenge and an opportunity. The Office of the National Coordinator for Health Information Technology (ONC) first published a 10-year vision for achieving infrastructure that was interoperable, followed by a roadmap. ONC then developed a framework for assessing progress on goals through 2024.17
ONC asserts that “nationwide interoperability has the potential to support a number of processes to help improve individuals’ experiences with the healthcare delivery system, reduce costs, increase efficiency of care, and improve health outcomes.”17
To achieve this success, there needs to be an increase in the number of EHR users across the healthcare industry that:
- Send, receive, find, and use electronic health information.
- Have electronic health information available from outside sources and make electronic health information available to outside sources.
- Use electronic health information to inform decision-making.
EHRs were once the latest innovation to the industry. Since then, they have evolved considerably, having a significant effect on institutions, providers, and patients. While the EHR has improved patient safety since the days of disjointed paper charts, faxed reports, and telephone messages, that improvement has brought with it a new set of challenges.
Looking to the future, it’s clear that though the industry is armed with powerful technology, it requires a human solution to help solve these challenges while relentlessly pursuing an enhanced patient experience, better health outcomes, reduced costs, and improved staff satisfaction.
References
- Leventhal, Rajib (April 2019). Research: first-year docs spend 43% of time interacting with EHRs. Retrieved from https://www.hcinnovationgroup.com/clinical-it/electronic-health-record-electronic-medical-record-ehr-emr/news/21076795/research-
firstyear-docs-spend-43-of-time-interacting-with-ehrs. - The Office of the National Coordinator (ONC) for Health Information Technology (October 5, 2017); Benefits of EHRs: Impacts of EHRs on Care. Retrieved from https://www.healthit.gov/topic/health-it-basics/benefits-ehrs.
- Busey, B. (December 2019). Interview on EHR Perspective. (V. Ferrari, Interviewer).
- Raths, David (March 2019). EHR-Related issues top patient safety concern list. Retrieved from https://www.hcinnovationgroup.com/clinical-it/patient-safety/news/21071783/ehrrelated-issues-top-patient-safety-concern-list.
- Leventhal, Rajiv (May 2019). Physicians, nurses give mixed review on EHRs improving care quality. Retrieved from https://www.hcinnovationgroup.com/clinical-it/electronic-health-record-electronic-medical-record-ehr-emr/news/21078776/physicians-
nurses-give-mixed-reviews-on-ehrs-improving-care-quality. - White, Jess, Healthcare Business & Technology (April 15, 2016), republished from Medical Economics; Avoid 4 Common Errors with Your Hospital’s EHR. Retrieved from http://www.healthcarebusinesstech.com/common-ehr-errors/.
- Raths, David (June 2019). Managing test results in EHR is no. 1 on ECRI Institute’s patient safety top 10 list. Retrieved from https://www.hcinnovationgroup.com/clinical-it/patient-safety/article/21085780/managing-test-results-in-ehr-tops-ecri-institutes-patient-safety-top-10-list.
- Leventhal, Rajiv (March 2019). Nurses far more satisfied with EHRs than physicians, KLAS report finds. Retrieved from https://www.hcinnovationgroup.com/clinical-it/nursing/news/21073897/nurses-far-more-satisfied-with-ehrs-than-physicians-klas-report-finds.
- Leventhal, Rajiv (March 2019). Patients give positive EHR feedback, though accuracy concerns remain. Retrieved from https://www.hcinnovationgroup.com/clinical-it/electronic-health-record-electronic-medical-record-ehr-emr/news/21072623/patients-give-positive-ehr-feedback-though-accuracy-concerns-remain.
- Patient interviews. (December 2019). Perspectives on EHR. (V. Ferrari, Interviewer).
- Longbreak, K. AMERICAN NURSE TODAY (July 2017). Focusing on the Quadruple Aim of Healthcare. Retrieved from https://www.americannursetoday.com/focusing-quadruple-aim-health-care/.
- Schulte, Fred and Fry, Erika, Keiser Health News (March 2019), republished from Fortune, Death by 1,000 Clicks: Where Electronic Health Records Went Wrong. Retrieved from https://khn.org/news/death-by-a-thousand-clicks/.
- Lippincott Solutions (September 2017). Moving from Triple to Quadruple Aim. Retrieved from http://lippincottsolutions.lww.com/blog.entry.html/2017/09/05/moving_from_triplet-uouA.html.
- NEJM Catalyst (March 2018). What is pay for performance in healthcare? Retrieved from https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0245.
- Britton, John, International Journal of Health Policy Management (May 2015); Healthcare Reimbursement and Quality Improvement: Integration Using the Electronic Medical Record, a comment in response to “Fee-for-Service Payment: An Evil Practice that Must Be Stamped Out”. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4529047/.
- Cerner (n.d.). Regulatory Services. Retrieved from https://www.cerner.com/solutions/regulatory-services.
- The Office of the National Coordinator for Health Information Technology (ONC) (n.d.); Connecting Health and Care for the Nation; a Shared Nationwide Interoperability Roadmap. Retrieved from https://www.healthit.gov/sites/default/files/hie-interoperability/nationwide-interoperability-roadmap-final-version-1.0.pdf
- The Office of Inspector General, CMS and Its Contractors Have Adopted Few Program Integrity Practices to Address Vulnerabilities in EHRs. Retrieved from https://oig.hhs.gov/oei/reports/oei-01-11-00571.pdf