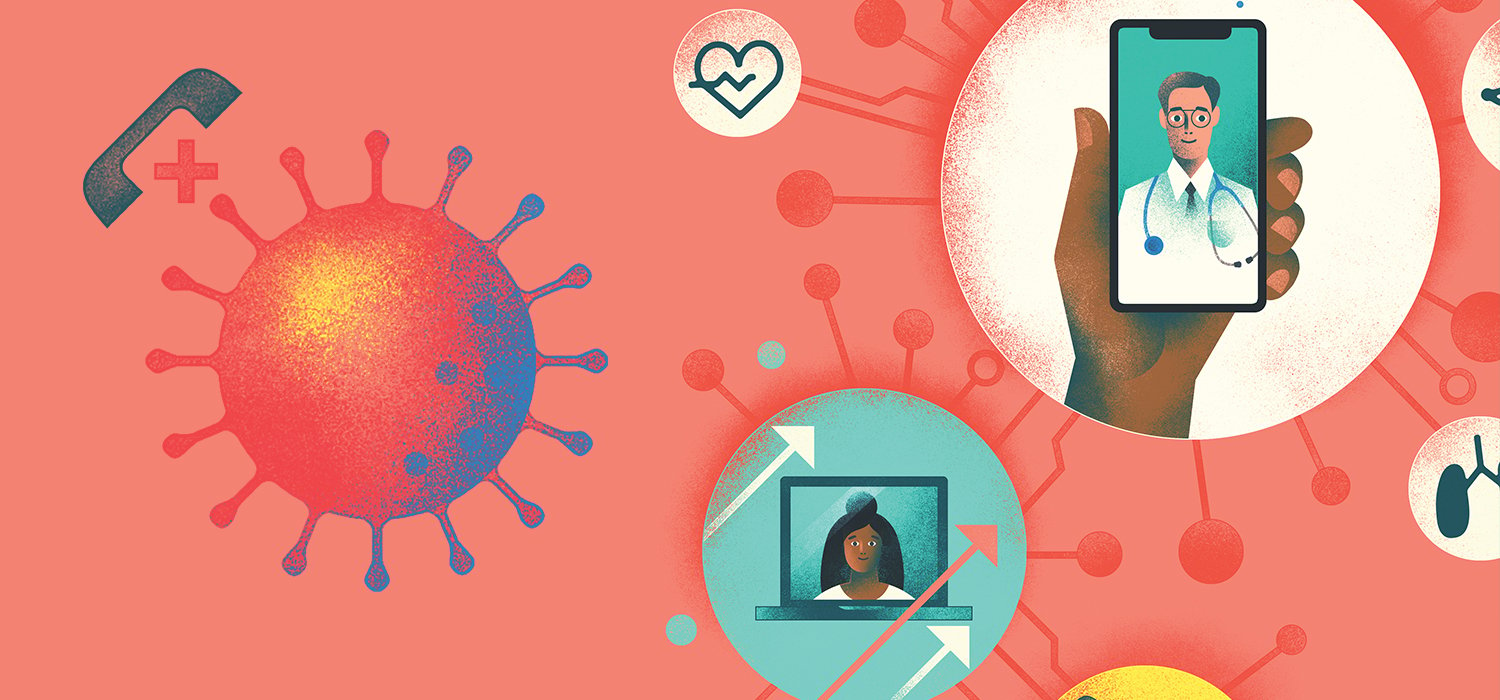
In response to COVID-19, policy changes paved the way for a rapid expansion of telehealth. As we reflect on the past year, we can learn from the opportunities and challenges that communications technology has yielded and take steps to prepare for what might come next.
In late January 2020, the first case of coronavirus was confirmed in the United States. Less than a month later, the CDC recommended that healthcare facilities and providers in areas affected by COVID-19 offer clinical services virtually. Following policy changes, telehealth expanded immediately and exponentially with unprecedented growth. There was a 154% increase in telehealth visits during the last week of March 2020, compared with the same period in 2019.[1]
The COVID-19 pandemic has been a launching pad for the accelerated growth of telehealth. Communications technology has been opened up in healthcare like never before, which has created both opportunities and challenges. Here’s an overview of where we’ve been, where we are, and where we are going with telemedicine and other communications technology.
Relaxed regulations that kickstarted the telehealth explosion
In March 2020, the Centers for Medicare & Medicaid Services (CMS) announced temporary relaxation and expansion of telehealth regulations, removing barriers to make telehealth opportunities accessible during the pandemic. These changes included:
- Physicians can be paid the same rate for telehealth services as in-person visits
- Patients can be home or in any other setting to receive telehealth services
- An existing patient-provider relationship does not need to be established to conduct telehealth visits
- Cost-sharing for telehealth visits can be waived or reduced
- Physicians licensed in one state are allowed to see patients in a different state
“Once those policies and regulations were lifted, patients were able to better access healthcare,” said Chelsea Johnson, MD, FAAP. Dr. Johnson was an advocate of telehealth prior to the pandemic and is currently the Associate Pediatric Lead at K Health: the most downloaded medical app that allows patients to chat with clinicians virtually anywhere.
“We can now interact with our patients so much easier, because we get paid, we can be at the right place at the right time, and because we don't have restrictions on things like waiting for a state license. It's been phenomenal being able to provide that care.”
How telemedicine is being used and who is using it
Nearly half of all patients (46%) say they use telehealth for some visits, compared to just 11% in 2019.[2] Virtual visits have slowed slightly since the beginning of the pandemic, but they are here to stay: 83% of patients say they are likely to continue using telemedicine after COVID-19.[3]
COVID-19 is responsible for telehealth’s rapid growth, but most virtual visits are non-COVID related. From January to March of 2020, 93% of telehealth patients sought care for conditions other than COVID-19. These telehealth encounters were mostly for adults ages 18-49, and 63% were female.1 The top three conditions patients sought telemedicine treatment for were:
- Allergy, ear, nose and throat
- Routine preventative care
- Mental / behavioral health / therapy3
Beyond patient visits, telehealth is also being used for better provider tools and collaboration. Many are using “store-and-forward” consultation applications, where medical data/images are sent to specialists who review and provide feedback at a later time. Remote monitoring tools that collect data such as weight, blood pressures, and blood sugar levels can be powerful in managing chronic illnesses like heart failure, diabetes, hypertension, and chronic obstructive pulmonary disease.

The rise of smartphone usage to streamline patient care
Other communications technology is being examined and innovated, and the stresses of COVID-19 has accelerated adoption. As demand for services increased due to the coronavirus, hospitals have turned to technology to help alleviate pressure on an already strained system.
“What COVID really revealed to us is that we’ve all got to get our acts together and get organized around our [mobile] strategy, because people die when we don’t get things to the right people at the right time,” said Kourtney Govro, Managing Director of KDG Innovations. Govro has 20 years of experience partnering with hospitals to design mobile strategies and has seen technology in healthcare settings evolve.
By 2022, 97% of nurses will use mobile devices at the bedside. Hospitals that have embraced mobile technology cite improvements including reduced cost of patient care and improved quality of patient care.[4] When healthcare workers have the ability to be more efficient communicators, they can more effectively work with patients and other care providers.
“There are certain things you have to do on your computer because of the way you have to enter information, but a lot of this information is going to be faster on your smartphone. And for allied health professionals, it's huge. Imagine if your pharmacy technician, or whomever, is assigned to a group of units. They may be assigned to the whole hospital and need to get information to the right space. Those kinds of communication pieces right now are super fragmented,” Govro said.
The drive toward patient-centered, collaborative care promises improved patient outcomes, but technology needs to keep up to be most effective at not only promoting team-based care, but also in addressing clinical healthcare worker burnout — which Govro says is the number one problem for 2021. “We need to be more collaborative to reduce workload. And we look at everything as workload,” she said. “From the physical act of entering a patient’s information into their electronic file to the emotional decision of which patient gets your attention at that moment in time… it’s all work, and it can feel like a heavy load.”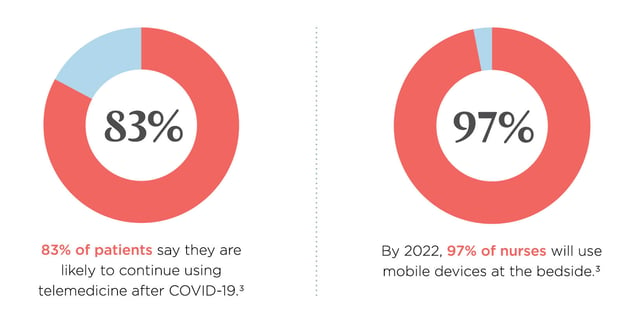
Benefits and challenges of telehealth
It’s been over a year since the world of telehealth was opened up in response to COVID-19. What have we learned in that time?
BENEFITS
Experts agree that telehealth is here to stay, and a big reason for that is because of all the benefits it has yielded, including:
- Improved adherence. 91% of patients agree that telemedicine would help with appointment and prescription adherence.3
- Expanded healthcare access. Virtual visits have allowed for on-demand healthcare access and allowed patients to connect with providers who might otherwise be out of reach.
- Patient satisfaction. Out of 1,000 telehealth patients surveyed, over 75% were very or completely satisfied with their virtual care experiences.[5]
- Control of infectious illness. Pre-screening patients for possible infectious disease can reduce exposure and prevent sick people from having to come to a healthcare office.
- Cost effectiveness. Telehealth can reduce overhead costs in the form of fewer exam rooms and less need for office support. Additionally, it creates the ability to see more patients, which can increase revenue.
- Comfort and convenience. Telehealth allows greater flexibility for both patients and providers. This can be especially impactful for those who are not mobile or for parents who stay home with children and have difficulty making it to appointments.
CHALLENGES
The rise of telehealth has improved healthcare access and connected clinicians and patients in new ways, but there are some growing pains to overcome (as one would expect with a sudden and drastic shift). Some of these challenges include:
- Cyber security concerns
- Limited access to adequate broadband services in rural areas
- Reimbursement issues (fee for service model)
- Lower technology use among older adults
- Limitations when certain examinations must be conducted in-person
- Liability concerns
Telehealth cannot completely replace in-person care, but it can provide care for both acute and chronic illnesses when a face-to-face visit isn’t necessary. Some challenges are policy-related, such as reimbursement, and many leaders in the healthcare space are optimistic that things are headed in the right direction.
“We are waiting to see how much we'll return to pre-pandemic restrictions and how much of it's going to continue to be as it were now, and hopefully change and improve access,” said Dr. Johnson.
Policymakers are currently introducing bills that would expand broadband access nationwide, which would remove a big barrier for rural patients. It’s likely that this is one of many developments that could impact telehealth in a big way.

Further advancements and changes to anticipate in the future
Time will tell what the permanent impacts of COVID-19 will be to healthcare technology. As we look to the future, some predicted advancements include:
- Increase of telehealth visits
- Expanded use of remote patient monitoring
- More focus on value-based care models of reimbursement
- Easier sharing of patient records (among providers)
- Increased use of smartphones for communication and monitoring
- Using AI to drive efficiencies, particularly as clinical decision support6
- More direct-to-consumer healthcare companies that challenge traditional healthcare models
Technology has come to the top of healthcare leaders’ priority list. Prior to the pandemic, a survey from the Center for Connected Medicine (CCM) revealed that just 26% of healthcare executives said that the shift to telehealth and virtual care was a top innovation priority … a number which has now jumped to 49%.[6] In the same survey, those who implemented quick, short-term solutions said they are looking forward to improving integration, infrastructure, and security for an updated telehealth strategy.
“I'm really looking forward to some of these changes, but it's going to take innovators and disruptors and people looking at the problem differently to impart new, creative solutions to way our healthcare system is,” Dr. Johnson said. “It will happen. It may not be this year, but more and more change is taking place in the right direction.”
How current and future healthcare professionals can prepare
In healthcare, as in any industry, advancement is one of the only constants. Although the lift of restrictions that enabled telemedicine to explode were temporary, it’s likely that telehealth is here to stay. Healthcare-related organizations and advocacy groups are pleading with Congressional leaders to make permanent changes, and current and future healthcare professionals should prepare themselves.
Healthcare educators are already incorporating telehealth training in their curriculum. In addition to being comfortable with technology, there’s a need for healthcare workers to learn good “web-side manner.” With virtual visits, some nonverbal communication is lost, and effective communication skills are needed to establish and maintain a strong patient-provider relationship. In the case of chat-based visits, such as those on the K Health app, it can be especially nuanced. Dr. Johnson said that you can impart empathy, even through chat, but that training is essential because it doesn’t come naturally.
Training solutions that help address this need are already available and are being used by healthcare educators and employers. Kognito, a company that is part of the Ascend Learning family, is a health simulation company that has incorporated telehealth visits into many of its simulated training solutions to better prepare clinicians for today’s healthcare environment. They also developed a “pre-visit checklist” to help providers better prepare for virtual visits.
“Our simulations do teach you what to say, but unlike most other training you’ll find, they also teach you how to say it,” said Gurnek Singh, Head of Product, Healthcare, Kognito. “It’s difficult to anticipate how you might come across the first few times, and you want to make sure that you’re overcoming some of the barriers of the technology to continue to deliver a strong, empathic, and caring type of provider visit.”
The adoption of telehealth and technology has been a silver lining of the pandemic. As we move to a new blend of virtual and in-person care, the future is unknown. But one thing is certain: the way people receive and prefer to receive care has changed. While in-person visits won’t vanish, it’s likely that the telehealth momentum the pandemic created will change the healthcare landscape for good.
Sources:
[1] Koonin LM, Hoots B, Tsang CA, et al. Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic — United States, January–March 2020. MMWR Morb Mortal Wkly Rep 2020;69:1595–1599. DOI: http://dx.doi.org/10.15585/mmwr.mm6943a3
[2] McKinsey COVID-19 Consumer Survey, April 27, 2020
[3] Doctor.com. (2020). Telemedicine Adoption in the Age of COVID-19 and Beyond. https://cdn2.hubspot.net/hubfs/3053445/Doctor_Telemedicine_Survey_Infografic.pdf
[4] Zebra. (2017). The Future of Healthcare: 2022 Hospital Vision Study. https://www.zebra.com/content/dam/zebra_new_ia/en-us/solutions-verticals/vertical-solutions/healthcare/white-paper/2022-hospital-vision-study-en-global.pdf
[5] Kyruus. (2020). Patient Perspectives on Virtual Care. https://www.kyruus.com/patient-perspectives-on-virtual-care-report-2020
[6] Center for Connected Medicine & KLAS Research. (2021). Top of Mind for Top Health Systems: Digital health priorities in the era of COVID-19. https://connectedmed.com/resources/research-report-covid-19-pandemic-shifts-innovation-priorities-at-health-systems/