Electronic health records (EHRs) gained widespread use in the mid-2000s, when the HITECH Act gave providers a financial incentive to switch from paper charts. Now, EHRs are ubiquitous in healthcare; a report from January 2020 found that 95% of hospitals use EHR technology.
As the demand for EHR technology has increased, so has the supply: in 2017, there were more than 1,100 EHR systems available to providers. No two EHRs are exactly alike, and each system has its own processes and quirks that staff need to master. Today, we’re going to examine the most common EHR mistakes your staff is probably making—and how they impact your bottom line.
Patient Misidentification
Patient ID errors are among the most common mistakes in health care. A 2018 report from Pew Charitable Trusts found that EHR match rates within facilities are as low as 80%; in other words, one out of every five patients may not be completely matched to their medical records. For records exchanged with an outside organization, the match rate falls to almost 50%—even if both organizations are using the same EHR.

The effects of patient identification errors can be calamitous; in some extreme cases, patient misidentification has resulted in patients undergoing the wrong surgical procedure. Most EHRs allow providers to add a picture to the patient’s record to lower the risk of misidentification, but these errors are still far too common, and the cost of this mistake can be enough to sink an organization.
Prescription Errors
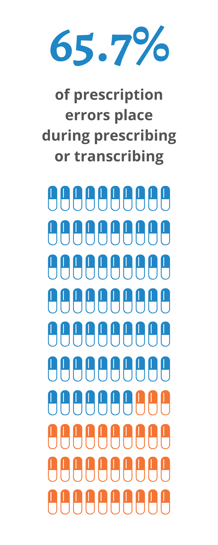
A recent study of 889 reported events found that nearly two-thirds of prescription errors (65.7%) took place during prescribing or transcribing. More than a third (35%) of all the reported incidents involved “high-alert” medications like insulin, anticoagulants and opioids, and another 16% involved antibiotics.
These errors can occur when:
- the wrong information is entered;
- the right information is entered, but in the wrong place, or;
- EHR flags/warnings for interactions or contraindications are overlooked
Prescription errors leading to patient injury or death are incredibly costly mistakes. Fortunately, additional training to ensure all users understand the proper processes can help lower your prescription error rate.
Billing Errors
Even under ideal conditions, medical billing can be complicated and laborious. Many insurers have unique claim processes, which requires your billing department to know how to navigate the nuances for each insurer. And if the claim isn’t filed exactly according to the payer’s instructions, the payment is likely to be rejected.
While some billing issues are the result of mistakes by your billing department, it’s equally common for errors to originate with staff entering the wrong CPT or ICD-10 codes in your EHR. Over time, these billing errors add up to a lot of lost money, both from unpaid reimbursements and from the time your staff will spend chasing down outstanding payments or resubmitting claims to insurers.
Cloning Patient Information
Thorough documentation is vital to good care, but most providers and staff will tell you that charting is one of their least-favorite duties. In this 2013 survey from Rand, many physicians cited “cumbersome, time-consuming data entry” as one of the biggest reasons why they don’t like their EHR. To cut down on charting time, it’s not uncommon for staff to clone, or copy and paste, patient information from previous encounters into the current encounter’s notes. It may save your staff a few minutes up front, but it creates a lot of extra work down the road.
Cloning patient info often leads to “note bloat”: charts filled with blocks of text that all contain the same basic information. A bloated chart makes it harder for providers to pick out relevant information and provide proper care. Providers can also have trouble accurately tracking the progression of chronic conditions. The copy-and-paste method often leads to subpar care:
if your staff aren’t thinking about what they’re typing, then they likely aren’t paying attention to details that could be relevant. And, any mistakes in the original note are carried forward to every subsequent note.

One audit found that 36% of copy-pasted notes ultimately led to diagnostic errors, which can be incredibly costly: diagnostic errors open your organization up to a lawsuit, and Medicaid and Medicare can reject claims if the notes are copy-and-pasted from a prior visit.
Which brings us to the biggest error of all:
Poor EHR Setup & Management
Of all the errors listed above, by far the most common is poor setup and management of the EHR itself. This might the most harmful mistake you can make, because the other errors on this list can more or less be contained; for example, an incorrectly-entered prescription will only affect that particular prescription. An EHR that has been poorly-implemented, on the other hand, will likely affect all of your organization’s processes.
On its own, the EHR is just a tool. A well-designed EHR can be customized and tweaked to make it more intuitive and easier to use, but instead of configuring the EHR to suit their needs, many providers and organizations make the mistake of trying to change their processes to suit the EHR. This leads to more mistakes and more (billable) time being spent trying to navigate the EHR.
How Can You Fix It?
Avoiding errors starts with setting up and implementing your EHR with the end-user in mind. Too many organizations place this responsibility solely in the hands of IT, when it should be a collaboration between IT, informatics, and clinical staff.
If the errors persist, your staff might need additional training, but finding time to retrain your entire staff can be a logistical nightmare. An easier and more effective approach is to invest in a certification for clinical staff members who use your EHR most frequently.
Having some EHR-certified employees will give the rest of your staff a permanent resource who understands your EHR, your clinical processes, and how the two fit together. That helps ensure your EHR is being used as intended, which means fewer avoidable errors—and fewer headaches.




